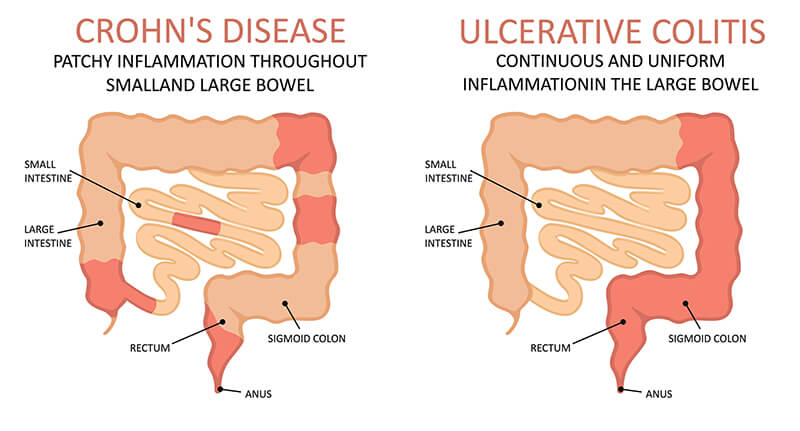
Inflammatory Bowel Disease (IBD)

SIGNS & SYMPTOMS OF IBD
These symptoms can vary from mild to severe, depending on how serious the inflammation is and where it is located. Furthermore, IBD can come and go, alternating between moments of flare-ups and remissions.
- Cramping and pain in the abdomen | This can be very severe, often before a bowel movement.
- Persistent diarrhoea | This can sometimes be mixed with blood, mucus, and pus.
- Anaemia | You may have low red blood count if you are losing blood, or not eating much.
- Weight loss | Your body may not be absorbing nutrients well due to the inflammation.
- Fatigue | You may be tired from IBD itself, anaemia, or night wakings from pain or diarrhoea.
CAN IBD BE CURED?
Unfortunately, there is no known cure for IBD. However, it can be treated long-term to reduce the severity and frequency of flare-ups, and reduce the risk of complications from developing.
HOW IS IBD TREATED?
Treatment for IBD is very much personalised to the individual, which can be determined by:
- Severity of disease
- Location of disease
- Past response to medication
- Side effects of medication
- Any comorbidities (other medical conditions that the person has)
TYPES OF MEDICATIONS
The first line of treatment for IBD is medications, which include:
- Anti-inflammatories | Decreases inflammation
- Corticosteroids | Keeps the immune system in check
- Immunomodulators | Modifies the activity of the immune system
- Antibiotics | Treats bacterial infection
- Biologics | Interrupts specific immune system signals to prevent an inflammatory reaction from happening.
WHEN SURGICAL TREATMENT IS NEEDED
Sometimes, medications alone may not be enough to sufficiently control the disease (symptoms and complications), in which case surgery may be necessary.
- After 30 years of disease, up to 1 in 3 with ulcerative colitis will require surgery
- Around 70% of people with Crohn’s disease eventually requires surgery
In the case of ulcerative colitis, surgery typically involves the removal of the colon and rectum, along with the creation of a “pouch” in order to facilitate bowel movements.
In the case of Crohn’s disease, surgery typically includes the opening up of narrowed/blocked portions of the small intestine; or a removal of damaged portions of the intestines and joining the remaining ends back together. In severe cases, a total removal of the colon may be needed.
If you have persistent symptoms of IBD, seek medical attention immediately. Our colorectal specialist will assess you closely and see you through a personalised treatment plan for long-term relief.